New aspects of breast cancerPersonal
Ana Luisa Villanueva
Chief Medical Officer Life, Health & Accidents
MAPFRE RE
Madrid - Spain






Our body is made up of many different types of cells. They grow and divide in a controlled way to maintain vital functions and the normal functioning of the body. Sometimes, this orderly process goes wrong. The genetic material, or DNA, of a cell can become damaged, producing mutations or changes that affect normal cell growth. When this happens, cells do not die when they should and new cells and structures appear, creating blood vessels for nutrition and developing a mass of tissue called tumour or cancer.
Breast cancer is one of the most important diseases present in the population of Western countries. It is the most frequent malignant tumour in females as well as the first cause of death, although its incidence varies depending on geographical areas. Differences are attributed to different lifestyles, environmental factors and diagnostic methods. The incidence of this type of cancer increases with the economic status, more than half of the worldwide cases come from developed countries.
According to the International Agency for Cancer Research, IACR, the incidence of this disease is higher after the age of 40, increasing after the fifties. While adjusted mortality rate is 18.5%, a clear downward trend has been observed. It is rarely present in males, accounting for less than 1% of all breast cancers. In these cases, there is often a delay in diagnosis since this possibility is not usually considered and progression of disease is faster than in women due to the lower volume of the breast.
Thanks to population based screening programmes, the incidence rate has increased and improvements in diagnosis and treatment have placed women survival rate above 80% in Spain, according to EUROCARE-4 study.
Biological aspects of the disease
Biological aspects define those processes and changes characteristic of tumour cells. It is important to know them to understand the development of the disease and the diagnostic methods used.
Breast cancers frequently display heterogeneity in phenotypic features such as:
- Cell morphology.
- Gene expression.
- Cell surface markers.
- Growth factors.
- Hormone Receptors.
- Metabolism.
- Angiogenesis.
- Motility.
- Proliferation.
- Immunogenicity.
- Metastatic potential.
- Metabolic reprogramming
Tumour cells have a different glucose metabolism than those of other tissues due to multiple cellular and environmental factors. This results in energy inefficiency and a higher flow of glucose. This feature is used in imaging diagnosis with a positron emission tomography scan (PET scan - Positron Emission Tomography).
This disorder results in a stimulus to cell growth, avoidance of apoptosis or programmed cell death, endless replication potential, increase in blood vessel growth or revascularization, tumour invasion, metastasis and escape from immune system. - Hypoxia or lack of oxygen
This feature is closely related to aggressiveness, progression and resistance to certain chemotherapeutical drugs, besides induction of various gene expressions through transcription factors. - Angiogenesis
This is the physiological process of developing new blood vessels from preexisting ones. While this situation occurs in normal conditions such as healing, it is an important phenomenon for tumour to develop and grow, not only in their original place but also in metastasis.
Tumours stimulate angiogenesis by releasing vascular endothelial growth factor. - Senescence – telomerase activity
Cellular senescence is defined as the limited capacity of cells to divide over a certain number of times. When cells avoid this process, they become immortal. This fact is related to chromosomal telomeres or specialised structures placed at the ends of the chromosome, which shorten with each cell division so that they reach a point where they cannot divide any longer. - Presence of associated macrophages
Until recently, the presence of macrophages in tumours was considered as a host response to the tumour. Now, we know they play an important role in tumour progression and invasion since their function is to phagocyte foreign bodies penetrating the body.
Among the functions of the tumour-associated macrophages there is the release of stimulating and activating factors to enhance vessel growth, migration and tumour invasion, immune suppression and protection against treatment. - Stem Cells
These cells account for less than 0.1% of tumour cells and are characterised by their self-renewal and production of stem cells able to differentiate into mature and differentiated cells. These cells are more resistant to the action of drugs, including chemotherapy and radiation therapy. They are currently used as therapeutic targets. - Metastatic potential – Bone metastases
83 per cent of patients with breast tumours have bone metastases, most often osteolytic (bone destruction), although 15 to 20% are osteoblastic (bone formation). Bone is involved by the interaction of the tumour with the bone environment by realising stimulating factors, which facilitates cell migration, adhesion of tumour cells to bone matrix, bone development and survival and proliferation of tumour cells in the bone.
Classification
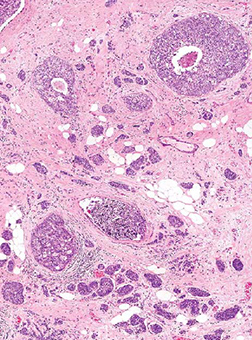
Histopathological assessment of breast cancer remains the main source of prognosis and most powerful predictive information and the main discriminating factor for specific adjuvant therapy.
Histological type and size of tumour, number of nodes involved and presence of metastases are key factor for tumour staging.
Current personalised management of breast cancer mainly combines a constellation of histopathological characteristics (tumour size, histological type and grade, number of lymphatic nodes involved and metastases) with other biological factors such as sensitivity to endocrine therapy, using biological parameters as the expression of hormone receptors for estrogens (ER), progesterone (PR) and HER2 (Human Epidermal Growth Factor Receptor 2), an important marker and cancer therapeutic target, especially for breast cancer.
| Stage | TNM |
|---|---|
| 0 | T0N0M0 |
| I | T1N0M0 |
| A | T0, T1N1M0 T2N0M0 |
| IIB | T2N1M0 T3N0M0 |
| IIIA | T0, T1, T2, N2 M0 T3N1 N2M0 |
| IIIB | T4 Any N M0 |
| IIIC | Any TN3M0 |
| IV | Any T any N M1 |
New classification – molecular classification
In recent years, several sophisticated genetic analysis techniques have been used to study breast tumour cells.
The relevance of this molecular classification is essentially based on improving treatment outcome, either by saving patients with good prognosis from side effects of unnecessary treatment or by choosing a subtype of patients with high chance of response to specific therapy.
Screening and diagnostic tests
According to the World Health Organisation (WHO), screening is the presumptive identification of unrecognized disease or defects by means of tests, examinations, or other procedures that can be applied rapidly. In breast cancer, these tests are vital for early detection, diagnosis and treatment of disease. Let us go through them.
Mammography
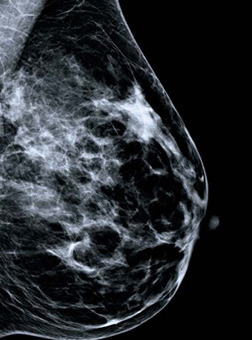
Mammography is the ultimate test in the diagnosis of breast cancer.
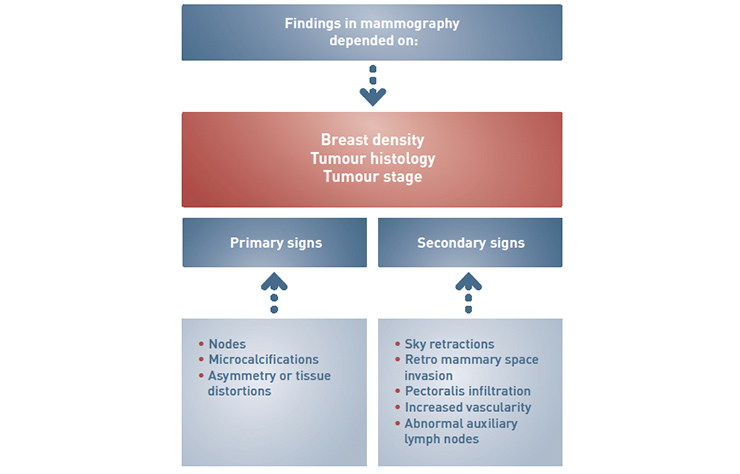
Before having a mammography, medical history and clinical findings should be analysed. This will help looking for images of any symptoms patients may refer or the reason of medical consultation. Therefore, imaging techniques should adjust to medical and clinical findings. The reading of a mammography requires a skilled professional, capable of correlating image data with that provided by the patient.
It is the most common and reliable method with a sensitivity close to 80 per cent that changes according to several factors: internal structure of the breast, type of lesion, morphology, place, breast volume and the quality of image.
Between 10 to 15 per cent of cancers with histological (tissue) analysis, have no radiological findings. Based on this fact, we need to have updated imaging techniques and if possible, complete the study with an ultrasound to increase sensitivity.
Mammography has achieved great technical developments, leading to improvements in diagnosis. New digital equipment and imaging manipulation techniques show us that the real warhorse is subclinical cancer, which early diagnosis and treatment ensure higher survival rates and a better plastic effect.
Imaging signs in breast cancer
New imaging techniques
Digital mammography or digital mammograph
This technique eliminates the need for film, taking advantage of digital technology for screen display, printing or filing. It optimises the image, providing a uniform thickness of the gland thanks to a better view of the subcutaneous tissue. It allows image manipulation, resizing, rotation, changes in brightness and contrast, storage in a CD or an electronic file or even printing in a high definition laser printer. Radiation from exposure is reduced, as there is no need to repeat projections.
Do not forget that a conventional mammography performed in optimal conditions can provide high diagnostic information even if printed on a film and the image cannot be manipulated.
This digital technique is especially useful in microcalcifications. These are the most common radiological diagnosis in carcinoma in situ, and very important in early detention. It gives a clear view of the shape and distribution of deposits, which are the most accurate determining parameters when malignancy is suspected.
Digital Breast Tomosynthesis (DBT)
This revolutionary three-dimensional technique let us have multi-slice individual projections, which later on are reconstructed in the different space axis, providing high resolution images. This implies a better reading of the tissue as it avoids image overlapping. It is especially useful in nodular lesions and unstructured areas.
Ultrasound
In a few years, this technique has gone from just being used to differentiate solid from cystic images to be an essential complement to determine the degree of suspicion of a radiological undetermined breast lesion. Among its advantages, the ability to evaluate the internal structure, orientation, morphology and margins of the lesion, both in fatty breasts as well as in dense ones where mammography is more limited.
- As initial diagnostic technique, it is used in young women under the age of thirty with symptomatic dense breast as well as in breast feeding or pregnant women.
- As a complement to mammography, it has an important role in breast with prosthesis, milk ducts study in patients with nipple discharge, negative mammography with palpable lump, women with risk factors and dense breast and in confirmed malignant cases with information on tumour size, skin and chest involvement, multifocality and multicentricity.
- Ultrasound is also a guiding tool in interventional procedures and pre-operative marking.
3D-4D Ultrasound
The implementation of a specific software to ultrasound technique provides a three-dimensional view of the tumour lesion to study its morphology and environment. This sophisticated software makes projections in several planes in space to assess, in terms of volume, the infiltration and deeper / superficial extension processing. It also helps placing the biopsy needle in the right position regarding the lesion.
Elastosonography
This recent technique is based on the principle of palpation of breast, providing an estimation of tissue strain and hardness.
There are currently two types of elastosonography:
Strain imaging, which identifies tissue stiffness and supersonic shear wave imaging, which identifies parameters such as maximum, mean or minimum elasticity (stiffness) of the studied structure.
This technique should be considered as a benefit to ultrasound, allowing confirming the ultrasound benign hypothesis thus reducing the number of unnecessary biopsies and providing guidance to low-risk patients for a better follow-up.
PET-TC
Positron Emission Tomography, better known as PET, traces metabolic process, which anticipates anatomical abnormalities. Tomography or Computerized Tomography, also known as CT scan, produces multiple images of crosssections of the body. The hybrid technique PET/ CT shows abnormalities in metabolic activity, providing qualitative and quantitative information for diagnosis, treatment and prognosis. In breast cancer, the spatial resolution is limited since it does not visualize lesions with a diameter less than 10 millimetres.
PEM
PEM or Positron Emission Mamography comes in use thanks to the limitations mentioned above. Although currently under clinical study, it is already giving better results than magnetic resonance.
This technique is used for surgical planning and monitoring of neo-adjuvant treatment response and relapse. The main disadvantages are cost and technical difficulty in handling the radiopharmaceutical.
Molecular imaging
Molecular imaging is defined by the American Society of Nuclear Medicine as the visualization, characterization and measurement of biological processes at the molecular and cellular level in humans and other living systems. This technique enables real-time monitoring, no tissue destruction and can be used in all phases of cancer management, from screening to most advanced situations. It is associated with all imaging techniques, from simple to complex ones such as computerised tomography, magnetic resonance, ultrasound and PET, as well as non-ionizing electromagnetic imaging.
How to treat Breast Cancer
Improved understanding of the mechanism of dissemination of the disease and the set up of population based screening programmes have resulted in an increase of early stage diagnosis and a very important development in treatment.
Oncoplastic surgery
Oncoplastic surgery provides surgical solutions to aesthetic breast reconstruction after mastectomy or during conservative surgery, as well as correction of any other sequelae from other treatments. It includes several mammoplasty techniques, breast reconstruction and risk-reducing surgery.
Breast reconstruction usually requires more than one surgery to get the proper aesthetic outcome. It may be indicated as prophylactic surgery in cases of high risk as well as in early or advances stages of disease, which will condition reconstruction to be performed in the surgical act or later on.
Hormonal Therapy
From studies to identify hormonal receptors we know that patients who are positive for both estrogens and progesterone receptors response to therapy in more than 50 per cent of cases. The greater the number of positive cells with a higher concentration of receptors, the better the chances of response. Depending on the case, it also helps reduce the presence of contralateral breast cancer.
Chemotherapy
Chemotherapy together with targeted therapy and hormone therapy are the current systemic therapy approach for breast cancer. The success of the treatment is based on reduction or ideal final elimination of any chance of relapse, which likelihood is directly related to therapy efficiency and inversely proportional to inherent tumour risk of relapse, determined by prognostic factors.
Elements in Therapeutic decision-making
Prognostic factors are those that provide information on the clinical outcome at time of diagnosis, regardless of the therapy to apply.
Prognostic factors require a series of features to be accepted as such. Their use should be simple, low resource consumption, reproducible, easily accessed and interpreted by clinicians. The only markers available meeting all requirements are: TNM classification, histological grade, menopause state, hormone receptor HR (expression), histological type and age.
The most well known current prognostic factors are:
- TNM classification.
- Tumour phenotype: tumour grade, hormone receptor status, lymphovascular invasion or HER2 expression.
- Age < 35.
At the XI Conference of the International Breast Cancer Group (IBCG) in 2009, it was agreed that decision-making based on predictive factors of treatment response was more appropriate than that based on risk prognosis factors. This way risk categories were eliminated to give way to therapeutic recommendations according to chance of response to treatment, hormone receptors (HR) and HER2 expression, as the only known predicting factors.
Radiation Therapy
It is advisable to choose a medical centre with the latest technology and a multidisciplinary team for a personalised therapeutic decision.
For more than thirty years, the usual standard therapy for patients with breast cancer, after conservative surgery, was external radiation therapy, involving daily radiation doses for a period of six weeks.
In the last ten years, two new techniques have developed; one related to duration of treatment, implying fewer fractions with higher doses, the other related to the amount of breast tissue exposed to ionizing radiation.
All this brings two new approaches:
- Partial Breast Irradiation (PBI)
PBI limits treatment to tumour bed and adjacent breast tissue, giving a margin of 1 to 2 cm, not including the whole breast. - Intraoperative Radiation Therapy (IORT)
This technique delivers an external single dose to different types of tumours.
Since the beginning of this century, a combined technique with the above mentioned has just started to be used: the Electron Intraoperative Therapy or ELIOT, which delivers a single radiation dose equivalent to the total fractioned external doses, after a wide resection or quadrantectomy, by using a mobile linear accelerator at the operating room.
Perspectives for Insurance
Continuous scientific developments, both diagnostic and therapeutic, involve not only an increase in life expectancy but also a better quality of life. For insurance purposes, this implies a constant update, not only in developing new products but also in the use of this new technology in the services provided in the policy.
Including in Health Care Insurance new tests such as screening, prognostic factors, genetics, all very useful for proper treatment, involve a significant increase in cost as well as an improvement in the quality of the offered services. This leads to a better position for the insurance company at the time of decision-making for the potential insured, a positive change in consumer’s perception and, in some cases, a rise in premium.
The crisis we are going through does not help investing in more sophisticated equipment but it is generating new products with more specific benefits, such as critical illness for specific types of cancer or screening testing related to other elements in preventive medicine.
For risk assessment in personal insurance, these developments imply a new approach for health questionnaires and test requirements. Early diagnosis together with therapy for advances diseases are providing a better risk classification, implying the acceptance of a higher number of cases with a premium adjusted to the real situation of the applicant.
The input of more accurate information to claims assessment will speed up the decision-making process and update the risk assessment process to make such decision easier.
The introduction of these scientific developments has brought a change in legislation. The predictive value of some of these new tests has made regulators to limit the use of the provided information, preserve the right to privacy and avoid discrimination.
Personal insurance has the challenge to integrate these changes to improve products and service and redefine risk classification.
Acknowledgements
Special thanks to Dr. Tejerina Centre for Breast Pathology for providing the necessary information to write this article.



