Dr. Rafael Matesanz
Director of the National Transplant Organisation (ONT)
Madrid - SpainPersonal
Rafael Matesanz was born in Madrid on 22 October 1949. He is married and has two children. He obtained his degree in Medicine and Surgery from the Madrid Complutense University in 1972 and he obtained his PhD in these specialties from the Madrid Autónoma University in 1979.
Specialising in Nephrology, he became the head of the Nephrology Department at the Ramon y Cajal Hospital in Madrid. He focused his clinical activity on comprehensive care of chronic renal insufficiency, from dialysis to transplantation. He is fluent in English, French and Italian. He was the driving force behind the creation of the National Transplant Organisation (ONT) in September 1989, and has been its director-in-chief from the beginning. The organisation, which belongs to the Spanish Ministry of Health, promotes, plans and coordinates all of the activities associated with the donation and transplantation of organs, tissue and bone marrow. Dr Matesanz is responsible for what is known internationally as the “Spanish Model,” for which Spain is ranked as the outright world leader in solid organ donation and transplantation.
From May 1996 to May 2000 he was the General Director of Health Assistance with the National Health Institute (INSALUD), head of primary and hospital care for 10 of the 17 Spanish Communities. From its creation in 1990 until October 2000 he was President of the National Transplant Commission. From 1995 to 2000 and from 2003 to 2005 he was President of the Council of Europe Transplant Committee. Between 2005 and 2007 he was Vice-President. From 1989 to 2001 he was the Secretary of the National Commission on Nephrology. From 2001 to 2008 he was the President of the National Commission on Nephrology. Between 1995 and 1997, he was Councillor of the European Society for Organ Transplantation (ESOT).
He has directed several national and international publications, has authored over 500 articles and of 100 chapters of books on nephrology, transplantation and health management. He has also been Director of Masters degree courses, advanced training courses and various post-graduate courses at several universities. He is a member of the board of several foundations, consultant and member of councils and committees advising several national and international bodies. He is Director of the Oncology Network of the Toscana Region (Italy). Between 2002 and 2004 he was an advisor to the Greek transplant organisation EOM; from August 2003 he was an associate of the Argentinean organisation of donors and transplants (INCUCAI). In 2005 he was an advisor in matters of transplants to the Institute of Medicine (IOM) -National Academies of Sciences- USA. Rey Jaime I Award for Clinical Medicine in 1999. He has the Great Cross of the Civil Order of Health, awarded in December 2006. He holds the “Order of Merit of Duarte, Sanchez y Mella” from the Dominican Republic, as officer. “Recognition Awards TTS (Transplantation Society) and Roche Award for Worldwide Impact in Transplantation 2008 Sydney (Australia).
From September 2004 until the present, he has been the national coordinator for transplants and Director of the National Transplant Organisation of the Ministry of Health. In 2010 he received the Prince of Asturias International Cooperation award as Director and founder of the National Transplant Organisation.






“We became the world leaders for transplants, and we still are”
The undeniable success achieved by the “Spanish model” in connection with transplants has gone beyond our borders and has caught on strongly in Southern Europe and Latin America. This success is based on a number of interrelated factors: people’s generosity, our own formalised ethical system, and a very professional management and coordination in the public sphere, which allows neither shortcuts nor unfair preferential treatment. A further key factor is a cost rationale resulting in far lower expenditure for treatment by transplant than for the alternative high-technology therapy needed to keep the patients alive. Being aware of events in this sphere means knowing one of the most dramatic stories of human achievement.
Since when have you been at the head of the National Transplant Organisation (ONT)?
Since its creation in September 1989.
What was the motor that jumpstarted the ONT?
It was something totally pragmatic. Nephrologists in Spain, as in other countries, needed to obtain organs to transplant to our patients on dialysis. Kidney transplants were performed much earlier than other organ transplants. I had seen how they went about it at the Ramon y Cajal Hospital in Madrid, and I realised that whether an organ was donated or not in individual cases depended on who was in charge. When I had the chance, I explained hospital by hospital and in the Autonomous Communities all over Spain, how the structural organisation should work and how we could simplify something that looked complicated.
Evolution was fast. It seems that from 1990 on, donations skyrocketed and everything was well organised.
People are generous, but what we have proved is that the problem with donations is one of management
In 1989 in Spain we had 14 donors per million inhabitants. We developed the system and donation began to be implemented increasingly throughout the country. It started more vigorously in the Basque Country, Madrid and Catalonia, as they were better structured, although the other Autonomous Communities followed. We became the world leaders in 1992 and we still are, twenty-one years later.
Being leaders in the management of transplants must incur a special responsibility given that many countries are trying to improve their capabilities in this field?
There are few body components that have not been transplanted and the frontier was crossed quite a long time ago, when we progressed from transplanting organs and tissues to transplanting composite tissues
I sometimes look back on what Spain has contributed to the world in this area, and it all begins with something very simple: donations do not come about spontaneously nor do they fall from the sky. It seems obvious, but this fact has had a major effect on the transplant situation in many countries, even those where they ran awareness campaigns to encourage organ donation - with only limited success. People are generous, there is no doubt about that, but what we have proved is that the main problem is how donation is approached and managed. If there are well-prepared professionals in the hospitals, who can explain the facts to the families, the process can be coordinated and the outcome is successful. Naturally, at this point there are countries that are replicating our model, like Portugal, which started about five or six years ago, and also Croatia, France, Italy and Belgium to a greater extent. In some countries transplant management is more complicated, because their health systems are very different from ours.
Are you talking about countries where organs are sold?
No, I am referring to countries with different healthcare systems. For example, it is very hard to adapt our model in Germany because private mutual insurance companies carry a lot of weight there. The United Kingdom has a very powerful national health service. They have examined our model and have adapted it. Strangely, doctors’ wages are far higher in the UK, which makes it that much harder for the UK to have our type of medical coordinators. In Latin America the number of transplantations performed is growing fast; the increase of 40% in the last five years is the highest in the world. To a large extent this is due to the fact that we have trained the professionals there. Right now we are training organ donation managers in Chile, Argentina, Uruguay, Venezuela, Colombia, Peru and several other Latin American countries. Australia has also adopted a system that is very similar to ours.
What system was in use before the ONT was founded? What led to the creation of this organization?
In order to maintain people’s trust it is essential that there is no possibility of giving preferential treatment, for financial or other reasons, when it comes to allocating organs
In the 80’s there was no organisational structure subject to normative guidelines. Each hospital organised its own transplants as best as it could. In my hospital, when we nephrologists needed organs, we had to handle the entire process intended to result in donation. We diagnosed the brain death of the donor, we spoke with the family, we obtained the organs, and we monitored the transplant patient. For heart or liver transplants, it was clear that the doctors specialising in those organ systems could not just go solo. So, we saw the need to have well trained specialists in each hospital, who could coordinate the process of donation and removal of the different organs, and who would always have appropriate teams ready to ensure that no organ that could be transplanted would be lost. This, along with communication and coordination with the ONT centre, made it all work.
How many transplants were performed per year at that time?
Over one thousand of different types: kidney, liver, heart and pancreas, among others, but almost a thousand were kidney transplants. Last year we reached 4,200. So, we have increased transplants fourfold. In addition, there has been an exponential increase in other forms of transplant, such as cell and tissue, which barely existed back then, though today thousands of them are performed. We can estimate that this year we will perform around 15,000 to 20,000 transplants of this type, including bone, bone marrow, umbilical cord, cells and corneas.
After these advancements, where is the frontier for transplants? At this rate, even brain transplants seem likely.
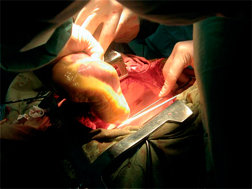
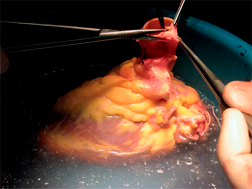
There are really few organs we have not yet transplanted. The frontier was crossed quite a long time ago, when we progressed from transplanting individual organs and tissues to transplanting composite tissues. Ideally, prophylactic medicine would prevent organ malfunction and the need for repair or replacement. But, when it is necessary and possible, parts can be replaced by means of transplantation. The new transplant philosophy centres on cell therapy, stem cells. The idea behind this is that, instead of replacing the part, the patient is given a series of cells capable of repairing the affected organ. Let’s say that this is the new frontier, but there is still a long way to go. The results are not yet satisfactory, and it will take us decades to get there. But it is an area with great potential.
In the last ten years composite tissue transplantation has advanced immensely: arms, legs, the face. Even uterus transplants have been proposed, but I think this is rather off target. In the near future, we will be seeing organ structures, especially hollow organs, covered by stem cells. For example, in recent years cadaver tracheas covered with stem cells have been transplanted. Since the stem cells are the patient’s own, there is no rejection. This works with hollow organs; the problem arises with solid organs, which are much more challenging.
What is the most complicated type of transplant?
Technically, the intestine is. Also a practice called cluster transplantation, which is really a multi-organ transplant involving the liver, stomach, intestine, pancreas and kidneys, for example. Multi-organ transplants in children are also very complex. La Paz Hospital in Madrid is one of the best centres in Europe for these types of operations. Transplanting seven organs in the same patient involves microsurgery, which is among the most sophisticated operating techniques.
Would there have been further advances in transplants if they were commercialised and were promoted by private health companies?
I do not think so. This is an issue that is linked to each country’s interests. For example, in the United States transplants are mostly organised by private medical companies. Countries in Southern Europe have clearly chosen transplants through the public health system, and I believe that this was a good choice because it entails transplantation of something that was selflessly donated by another human being, be it organs, tissue, marrow, cells or bones. In order to maintain people’s trust, it is essential that there should be no place for preferential treatment when it comes to receiving the organ, for financial or other reasons. We are at the top of the ranking on transplants in the world because we have maintained a cast-iron system, meaning that we do not admit any type of shortcuts when it comes to finding donors. And this is incompatible with private medicine. There are numerous examples all over the world. As soon as people see that wealth provides easier access to a transplant, the whole system collapses. On the other hand, given the public nature of our system, which is intended for everyone, we know that we are in effect constantly subjected to audit, and that our ratings of transplants and donors are well known. This is very important because we are dealing with human lives here. We are deciding who lives and who does not.
Is the profile of the Director of the National Transplant Organization more technical than political?
I think so. If we had to define what we do, I would say it is managing people. For a long time, we had a centralized national healthcare budget, but now, with a health system that is as decentralized and non-pyramidal as is Spain’s we cannot manage anything directly, not in Andalusia, Madrid, Catalonia or in any other autonomous region. We can only coordinate very large numbers of people, who are not even specifically assigned to the transplant system. When we coordinate several agencies, we work with large teams: surgeons, coordinators, clinical staff, nursing staff, laboratory technicians, couriers, airport staff and many other professionals who are not under our direct supervision. We have developed protocols to motivate and train them in their work. Again, what we manage is people. And all of this, with a budget under four million Euros.
Despite the fact that the health system in Spain provides full coverage, many people also have private insurance. Who do they go to when they need a transplant?
People usually go to the public health system, if that is the one that works. In the case of large groups of civil servants, such as MUFACE1, the person who requires a transplant is put onto our common list, just like any other public health system patient. It could not happen any other way, and once the procedure is performed and the cost calculated, the bill is sent to their insurance.
Longer lives
What is the average life expectancy of a transplant recipient?
That depends more on the patient than on statistics. Spain has a huge number of elderly inhabitants and we are performing transplants in people aged over seventy. We obviously cannot expect a further life expectancy of 25 to 30 years for those patients. At present, the world record for post-kidney-transplant survival is held by a woman who received her replacement kidney in 1960, in Boston (USA). This means that she has survived for fiftytwo years thanks to a kidney donated by her sister, and both of them are fine. In Spain, the first kidney transplants were performed in 1964. Now we have quite a few people who have lived for over forty years with a transplanted kidney. In general terms, survival rate for this type of transplant is fourteen years if the kidney comes from a cadaver and over eighteen if it comes from a living donor.
Is it harder to determine survival rate for recipients of other organ transplants?
The scheme would not work the same in the private sector. Part of its success has been achieved because people, donors and patients, firmly believe that this is a system belonging to everyone and for the benefit of everyone
Every case is different. For example, in Spain we have patients who have lived for over 25 years with a transplanted liver, and there are many cases in the world at large of such patients who have survived for 30 years or more. The situation is similar for heart transplants, though those who received replacement hearts in the pioneering days did not have such good surgery or anti-rejection drugs, and this all had an influence, but it is also true that both the donors and the patients were much younger. Now age is not an impediment to receiving a transplant.
In a climate of crisis like the current one, is it possible and necessary for the system implemented by the ONT to be maintained?
Sustainability of the system is fundamental. Could the scheme be transferred to the private sector? It would not work the same. It has proved successful partly because people, donors and patients, firmly believe that this is a system belonging to everyone and for the benefit of everyone.
Has anyone ever questioned the ONT?
Spain is the European country with the highest number of stored umbilical cords, and between 17,000 and 18,000 transplants have been performed, saving the lives of many children and adults with leukaemia or other cancers
Not in so many words. We are an entity within the public sector that has its budget stable. But we have difficulties when general health service budgets are reduced. The problem then is not with the health system or with the transplants but with the whole of society. To perform transplants, resources have to be mobilised, and in times of economic cutbacks this is harder to do. In recent years, many of the people who work in the transplant area have seen their pay drop by 20%. We have expressed our concern, because there is an essential fact to bear in mind: when a person who needs regular dialysis has a kidney transplant, this translates into cost savings.
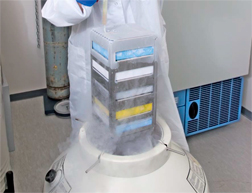
What is being done regarding blood banks and usage of blood and stem cells from neonatal umbilical cords?
Now age is no impediment to receiving a transplant
These are two different things. The cells in the umbilical cord are blood stem cells that yield blood. In the 80’s and 90’s a universal strategy was developed for storing umbilical cord stem cells. Today there are more than 500,000 umbilical cords stored in public banks around the world, and in Spain we have over 10% of these cords. Our country is also the leading country in Europe, regarding blood units of umbilical cords being stored, and worldwide, we are only behind the United States. Between 17,000 and 18,000 transplants have been performed, saving the lives of many children and adults who had leukaemia or other cancers. The harvesting of these cords is fully justified. What is not so justified is to keep the cord for oneself, which is what the private sector offers. There is a reason for this: if one of those children or adults whose umbilical cord has been stored contracts any of the diseases that make it necessary to resort to the cord, but it is a congenital disease or of genetic origin, you have to discard your own cord. This means that keeping the umbilical cords in private banks must be analysed from the financial perspective because the statistical probability of having to resort to it, and that it will be useful to you, is very, very remote.
But that is a decision for each individual. What does make sense is the system of allogeneic banks (where donor and recipient are different people), and these are public banks available to everyone. We have eight such banks in Spain. The cost of storing the umbilical cords in private banks is high but their medical usefulness is unclear. It could be that in the future, in 30 or 40 years, there will be other types of treatments that will totally supersede the purpose of these banks today.
The European Union and the European Council
have specifically recommended through several
documents the total or partial adoption of the
Spanish model for transplants: Meeting the
Organ Shortage: Current status and strategies for
improvement,
http://www.ont.es/infesp/DocumentosDeConsenso/
Meeting%20_the_organ_shortage.pdf
An island within the Spanish Health System
Who does the National Transplant Organisation come under in organisational terms?
It has always been under the Ministry of Health, and it is located in the Instituto Carlos III, which was incorporated in the eighties and is conceived as a research entity within the overall health system. For a long time, we have been like an island in the Institute’s premises, even though we are not part of it. The reason why we are here is because we are active 24 hours a day. Our call centre operates at all times, every day of the year, and this makes it quite difficult for us to occupy offices in the Ministry.
How much does it cost the Spanish taxpayer to maintain the ONT?
We have an annual budget of 3.8 million Euros, which includes the works developed by the ONT but not the performance of transplants.
That does not seem to be too much.
Transplant costs are quantified. There are probably few things in healthcare that are subjected to such close scrutiny. To understand the cost/benefit ratio of treatment by transplant, we can look at the classical kidney transplant. When a person has renal insufficiency there are three options: dialysis, a transplant, or being left to die. Of course, depending on the country, the last option is not even contemplated. The average cost of dialysis in the European Union, everything included, is around 50,000 Euros per year. For the person who has received a transplant the cost is more or less the same for the first year, but afterwards it goes down because, if there are no complications, care is limited to the medication alone. This means that the cost of maintaining a kidney transplant recipient is 5,000 to 6,000 Euros per year. But for patients receiving dialysis, the costs just go on rising. The more complications the patient has, the more it costs. In view of this, the outlay for a transplant is recouped within the second year. This is one of the reasons why transplants are performed globally. Spain is the only country in the world where we have the same number of dialysis patients as transplant recipients. If they were undergoing dialysis, it would cost the public coffers double the amount.
1 MUFACE: Mutualidad General de Funcionarios Civiles del Estado (General mutual health insurance of State officials) http://www.muface.es/



