Bioethics, science and technology intervention on life. Principles and ScopePersonal
Ana Luisa Villanueva
Chief Medical Director, Life, Health & Accidents
MAPFRE RE
Madrid - Spain
The concern about misuse of medicine and scientific knowledge dates back to ancient times. Practising this profession implies dealing with life, healthcare and death, and always had an ethical dimension.



For centuries, doctors themselves were those who after their experience and common sense made the necessary competences and honesty requirements, to work in hospitals or be part of a professional society or academy, come true in the form of oaths or codes. Medical Ethics has mainly expressed as medical deontology and its first and best well-known consequence is the Hippocratic Oath (5th century BC).
The term “Bioethics“ comes from the combination of Bio-Ethik (Greek “bios”, life; “ethos”, behaviour) and was coined by the German protestant pastor, theologian, philosopher and educator, Fritz Jahr, who in 1927 published an article reviewing the relationship of humans to plants and animals.
The American biochemist, dedicated to oncology, Van Renselaer Potter, used the term “Bioethics“ in 1970 in his article “Bioethics: The science of survival”. In 1971, he published “Bioethics: a Bridge to the Future” where he expressed a set of concerns about medical practice and the use of technology.
Bioethics projects on the beginning of life and its planning, cure and treatment of diseases and the end-of-life stages. The concepts it moves around not only have ethical implications but scientific, political, social, economical and legal ones. Therefore, bioethics is a multidisciplinary discourse. It aims to provide clear and conclusive rules to what (ethically) shall and/or should be done to every problem or bioethical raised discussion and to reach consensus on the present and future bioethical issues where disagreement exists or might exists.
For Daniel Callahan, founder of the Hastings Center, one of the factors that has most contributed to the acceptance of bioethics studies in the United States was leaving the theological or religious analysis to focus on secular bioethics, more interested in seeking consensus to cultural and ideological diversity. He defines the minimum ethics as the least common moral denominator in a pluralistic society, the minimal ethical level required; allowing society to legislate on matters not only at state level but also globally, whereas the maximum ethics refers to the maximal ethical optional level for our particular ideas of moral perfection.
Basic principles in Bioethics
Bioethics is no exception to ethics since its principles are the same as those ruling in any other human environment, they just have to adapt to the procedures of the activity.
The three Classic or Fundamental Principles in Ethics are:
| Classical Ethical Principles | Principles in Bioethics | |
|---|---|---|
| Main | Secundary or complementary | |
| Respect for autonomy |
Respect for autonomy Information |
Paternalism True-telling |
| Dignity |
Beneficence Nonmaleficence Non-instrumentality |
Restricted utilitarianism |
| Universality or equality | Justice and fairness | Difference |
- The Principle of Respect for Autonomy. This principle entails a third person not to make a decision for another one that cannot make it.
- The Principle of Dignity. This principle compels to respect individuals; requiring not causing harm to others or use them as a simple means.
- The Principle of Universality or Equality. This principle implies not giving a different treatment for those in the same situation.
“A physician in no case will leave a patient who needs his medical assistance in case of attempted suicide, hunger strike or refusal of treatment. He will respect the freedom of the competent patient. He will treat and protect the life of those who are not able to do so, asking for legal support when necessary” Code of Ethics and Medical Deontology, art. 9.4
The basic principles of bioethics build in ethical criteria for decision-making in clinical practice and biomedical and biological research, which achieved broad consensus around research using human embryos, experiments on humans, euthanasia, transplantation, gene therapies, refusal of medical treatment and allocation of health care resources among others.
The bioethics theory of a decent minimum care dominating the contemporary discussion is expressed in 1979 by Tom L. Beauchamp and James F. Childress (Kennedy Institute of Ethics, Washington, USA). In their book “Principles of Biomedical Ethics”, they present four basic principles in medicine:
- The Principle of Respect for Autonomy requires respect for self-governance of the patient. This principle has generated the Spanish Act 2002 of Patient Autonomy.
- The Principle of Beneficence or the duty to be of the benefit of the patient and strive for the best possible alternative both in practice and in research.
- The Principle of Justice or Fairness or the duty to promote fairness in treatment, distribution of benefits and research.
- The Principle of Nonmaleficence (primum
non nocere) or the duty to avoid doing
harm, imposing respect to physical and
psychological integrity of the individual.
Within this principle fall two classical
principles in medical ethics.
- The Principle of Proportionality in Treatment requires the gained benefits to compensate the harm or risks caused by medical intervention, such as the removal of a part of the body to save the live of the patient.
- The Principle of Double effect or Indirect
Voluntary refers to lawful medical act with
two effects, one good and another one
bad. Having no better alternative, it is
performed seeking for the positive effect,
even if, as a side and involuntary effect,
the negative effect occurs. This would be
the case in terminal patients under pain
relive therapy, even if this procedure
shortens their life.
Two more Basic Bioethical Principles can still be added to the Classical Ethical Principles of Respect for Autonomy, Dignity and Universality or Equality:
- The Principle of Information, closely related to Respect for Autonomy, express the duty to inform individuals of all possible aspects that affect or may affect their health.
- The Principle of Non-Instrumentality, which is another form of the principle of dignity and expresses the duty to treat individuals as ends, not merely as a means.
There could be the case where personal circumstances do not let the individual make a decision or conditions for the application of the principles of respect for autonomy, information, dignity and equality cannot be considered.
In this case, the Secondary or Complementary Principles are proposed:
- Principle of Paternalism. It is allowed to make a decision involving the life and health of another one if the latter is in a disabling situation and the action grants a benefit to the individual.
- Principle of Truth telling. It is allowed to hide information about health to an individual if, by doing so, his person is respected or enables a study to which there has been a previous consent.
- Principle of Restricted Utilitarianism. It is allowed to take an action that involves a benefit to the individual if this provides a significant benefit to another or others, there is a previous consent of the person involved and the action is not degrading.
- Difference Principle. It is allowed to treat a person in a different way if the difference in treat is based on a circumstance that grants significant benefit to another or others and can be rationally presumed that the involved individual would give consent if he could.

Scope
Bioethics in Human Reproduction
The Oviedo Convention in 1997 expressly prohibits the creation of human embryos for research purposes and cloning for reproduction but allows countries to research and experiment with already existing embryos in vitro while ensuring their adequate protection
The Principles of Beneficence and Nonmaleficence, as well as that of Respect for Autonomy, project on human reproduction in a very intense and controversial way. The latter has gone from being an event to a voluntary and deliberate act, which makes those involved the only responsible for it. Women liberation, mainly regarding sex, contraception, abortion and assisted conception represent a group of cultural and technological factors that have contributed to this change.
Deciding when the embryo becomes an individual will determine the solution to the conflict between respect for the reproductive autonomy of the parents and the obligation not to harm the individual as in the principle of Nonmaleficence. Around this concept, new questions show up, such as using frozen eggs and embryos, what to do with them after some time or the number of embryonic transfers.
Bioethics in Heath Care Relationships
Moral rules demand requirements that possibly may enter into conflict with other legal ones. This discrepancy in the doctor-patient relationship may generate the following situations:
Conscientious objection
The objector disobeys those rules that represent an obligation whose performance is not compatible with one’s own conscience.
Refusal of medical treatment
It may be considered that it only serves to prolong life unnecessarily (and maybe the agony) or the refusal seriously endangers health or the life of the patient, and there are no other available alternative therapies. Both the Council of Europe Bioethics Convention and the Spanish Act of Patient Autonomy, consider the patient’s right to refuse treatment. The latter has recognize the value of the “Living Will”, also named “Advance Directive or Advance Decision” which grants the patient the right to reject or stop treatment in case of certain situations where circumstances may not allow him to do so.
Limitation of Therapeutic Effort or LTE
It refers to not starting certain advanced technology measures that may seem extraordinary or disproportionate to the therapeutic purpose in patients with poor prognosis and/or quality of live.
There are two possibilities:
- Not starting certain measures.
- Withdraw a previous treatment.
The main ethical problems that arise are:
- A non-indicated LTE, which usually comes from the refusal of a measure in the fear of not having the choice to withdraw it later on.
- Professional obstinacy, opposite situation to the above mentioned.
- Refusal of an indicated LTE by relatives, due to a wish to maintain life at any costs, denial of death or guilt feelings.
| Primary functions | Secondary functions |
|---|---|
|
|
Informed Consent
This document is a new way to understand doctor-patient relationship and decision making in medicine. It is currently an ethical requirement and a right recognized by law in all developed countries. Its presence involves overcoming paternalism, giving patients access to control information and decision-making.
Ethical Committees in Health Care or Clinical Ethical Committees (CEC)
Conflictive ethical situations in clinical practice are quite numerous, for this reason, healthcare institutions have a CEC. This is a multidisciplinary group made up of physicians from different specialties, nurses, nursing assistants, customers, lawyers and other people related to the centre, all of them with a background in bioethics. This is a nonexecutive advisory board, so their decisions are non-binding. Protection of patient’s rights, coordination of methods for decision-making in ethical conflicts (Clinical Ethical Guidelines and Advice) and education in Bioethics for in-house staff are among their main tasks.
End-of-life Bioethics
In the last years, due to organ transplantation, legislation has moved away from the strict brain death criteria as being the only criteria to determine the death of the individual. The reason behind is “organ donation in asystolia”, that is to say, use the organs of someone who suffered sudden death, circumstance which does not follow the protocol for brain death.
Spanish Criminal Code defines euthanasia as a crime, same type as extenuating circumstances in cooperation to suicide. This law states the penalty of imprisonment from two to five years for those cooperating in the necessary actions for suicide and with a penalty from six to ten years if cooperation leads to death. There is not any sentence in Spain to date
When talking of the end-of-life, some questions come up: should we avoid death? Do we have to live? These questions take us to a very up-to-date issue: Euthanasia.
Euthanasia, from Greek eu - “good” and thanatos - “death”, is the central point of one of the deepest social demands of our time, to die in good conditions. Disagreements on its definition deal with:

Mode of behaviour: action or omission
When the term refers to taken actions causing (directly or indirectly) the death of person suffering from an incurable, painful and severe disease, it is called euthanasia or active euthanasia. It has a negative connotation and is very much denounced.
When it comes to not taking, withdraw or avoid the measures that could artificially prolong the live of the individual, it is referred as ortothanasia or passive euthanasia. It is considered benevolent and used when life is fatally approaching the end.
Nowadays, medical advances allow prolonging life to unthinkable limits. In this environment of possible therapeutic obstinacy, passive euthanasia shows up as a sort of disease management and used when these advances can cause useless suffering. It is not enough to have a serious physical illness and a very poor quality of life but it has to be irreversible.
Person’s will
Euthanasia is sometimes identified with an involuntary behaviour that is not requested by the one who is dying. On the other hand, there are times when it is identified with a demand for dying.
Motivation and circumstances
The motivation behind this behaviour is, on one side merciful, to avoid suffering, and on the other side resembles murder, genocide or extermination.
Bioethics in Research and Experimentation
Jean Dausset, 1980 Nobel Prize in medicine and President of the Universal Movement for Scientific Responsibility, defined in 1991 the “freedom of research” as key for development of knowledge and justified by the right of humanity to know. In the case of Research in Biology and Medicine, it is also supported by the benefit of their results and the impact they may have on health and welfare of the people.
The above mentioned could be called “external limits”, that is, what could be studied. There are also some “internal limits” that require addressing two issues: human experimentation and research on human embryos.
The World Medical Association Declaration of Helsinki in 1964 was the first document including ethical criteria and guidelines to protect those individuals participating in clinical research.
In 1982, the CIOMS (Council for International Organizations of Medical Sciences) issued the International Ethical Guidelines for Biomedical Research Involving Human Subjects, emphasizing the need for developing countries to protect individuals from experimentation. The Principle of Justice is applied in this case, so research with no therapeutic benefits cannot be carried out at the expense of vulnerable subjects and those with therapeutic benefits cannot exclude this very same population.
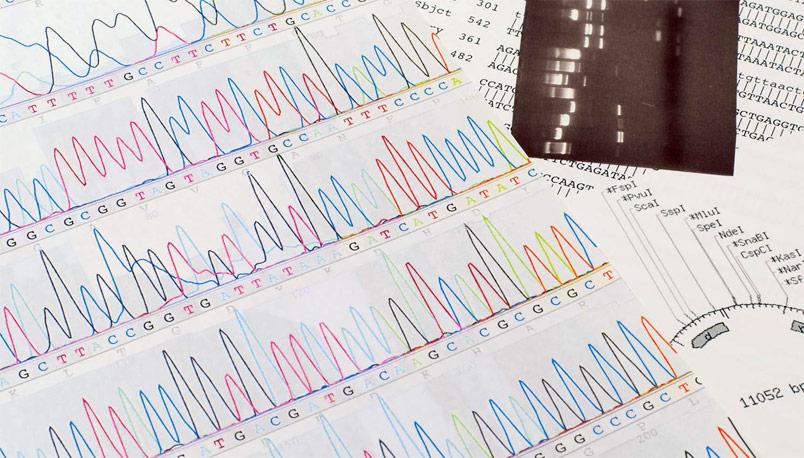
Regarding the human embryo, we know today that it carries stem cells. Research on these cells offers great hope for the cure of many currently incurable diseases. Therapeutic cloning or somatic cell nuclear transfer to create stem cells from a clone embryo to develop tissue or organs for selftransplantation is one-step ahead.
The main ethical problem arising from therapeutic cloning is the instrumentalization and loss of value of the human life. The embryo is created for the sole purpose of research or developing treatments, only as a simple source of biological material, which downgrades its moral status transforming it into a means to an end.
Bioethics and brain or Neuroethics
The term is coined in 2001 from an event gathering neuroscientists, bioethicists, psychiatrics, psychologists, philosophers and professors of Law and Public Policy in San Francisco, USA. It is understood as the relationship among ethics, neuroscience and clinical practice, keeping in mind the freedom and responsibility of the individual, the biological bases of the social behaviour, decision-making factors, consciousness, memory, education and learning process, social pathology, privacy, prediction of future brain diseases, pharmacotherapy, ethical changes in Alzheimer’s disease and other dementia, surgery, gene therapy, neurotechnology, brain implants, cyborgs, science dissemination and scientists training.
Brain implants are implants placed on the brain to restore lost or impaired brain functions. Cyborg, short form of cybernetic organism, refers to a person carrying a cybernetic device to enhance capabilities of the organic part
In this section, we cannot forget the weight of the widely used Living Will, also named “Advance Directive or Advance Decision. In 2007, Spain published a Royal Decree establishing a civil register for such wills. Patient’s medical record has just started to include it. This encloses those diseases or situations for which there is no wish for vital support to maintain life. There are relatively clear cases such as deep coma and others much more difficult such as Alzheimer’s disease.
Bioethics and Insurance
Most of the above issues, so far, have implications for the insurance world.
In risk assessment:
- The Principle of Respect for Autonomy in
the Health Declaration. Article 10 of the
Spanish Insurance Contract Act indicates
the duty of policyholders to declare their
health state according to the questions
submitted by the insurer. The insured is
free to answer these question and the
answers shall be true and within their
knowledge.
It is in the hands of the insurer to prepare the questionnaire and set the necessary medical tests to known the applicant’s health state.
The New medical and diagnostic advances, mainly in genetics, have introduced the concept of predictive testing.
Predictive testing shows the risk of developing disorders that may not yet be present. If we consider this test in an asymptomatic individual, we shall also consider the limitation of the result, since there are other non-genetic factors, mainly from life style and interaction with the environment that may influence the outcomes of prediction.
Nowadays, any information related to genetic testing is not used in risk assessment. Nevertheless, advances in genetics are going to have a great importance in treatment and diagnosis of diseases and will fully affect life and health insurance. - Informed consent for the tests to be performed.
- The right to be informed of the results of these tests. An extreme case would be the duty to inform the applicant of a positive HIV testing.
- Non discrimination, again related to genetics, in both prescribing and asking for results and the inability to use that information for risk assessment.
- The Principle of Fairness, that does not mean equality. Each insured pays a premium according to his risk factors - fair rating.
In health insurance, it fully involves covers and services:
- Diagnostic methods and new medical developments, such as in vitro fertilization, stem cells therapy, genetic testing and pharmacotherapy.
- Informed consent for all procedures that require one.
- Ethical Committees to provide guidelines.
- Fairness in treatment with no discrimination.
- Information available to insureds/patients.
- Maintaining Confidentiality.
- Clear statements on decisions at the end-of-life.
- Healthcare policy and strategies according to minimum and maximum ethics.
- Principle of Respect for Autonomy, considering disability or level of dependency.
Long Term Care/Dependence Insurance providing any kind of services shall consider all bioethical principles. The intense relationship between medical knowledge and life makes it necessary to build a solid base to understand, respect and treat the individual, always looking to maintain their dignity and quality of life.
To think about
- Bioethics let us address how scientific and technological advances involve life, death, health and the environment.
- The step where the embryo becomes a foetus is one of the main open questions involving decision making in both reproduction and research.
- The thin line between life extension and death invites the individual to think over his future and express it on a Living Will or make his beloved ones party to his decisions.
- We must find a balance between science and life in order to maintain a proper relationship with the environment.
Bibliography
Bioética, principios, desafíos y debates. Pablo de Lora y Marina Gascón. Editorial Alianza Editorial SA Madrid 2008.
Bioética: de la globalización a la toma de decisiones Docencia Universitaria. Editorial ADEMAS 2012.
Manuel Atienza, “Juridificar la Bioética” 1996 y “Bioética y Derecho” Lima-Bogotá, Palestra – Temis, 2004.
Council of Europe Bioethics Convention.
Spanish Act of Patient Autonomy.



