From traditional to modern medicinePersonal
Ana Luisa Villanueva
Chief Medical Officer Life, Health & Accidents MAPFRE RE
Madrid - Spain





The medical concept of disease has undergone great changes along history and helped understand the development and structure of society. Diseases suffered by the population are different upon the historical, economical, social and geographical moment. The cause of death along history changes according to different types of disease.
For most human history, life expectancy has been changing from 25 years from our huntergatherer ancestors, 37 years for residents of England in 1700, 41 years in 1820, 50 years by the early 20th century up to 77 years nowadays. This increase in life expectancy or decrease in mortality are explained by the near elimination of deaths from infectious diseases, most common cause of death up to mid-18th century. The improved nutrition and economic growth, as well as emerging public health measures from the mid-18th century to the mid-19th century and the delivery of clean water, waste removal and initial advice about personal health practices from the mid-19th century to the early 20th century. Since the 1930s, mortality has been reduced thanks to advances in medicine, primarily by vaccination and antibiotics and later by the new therapies that characterize modern medicine.

A quick review of the evolution of medicine
For Galen, disease had an Aristotelian philosophical background and a humoralist concept of the body
Galenism represents the prevalent medical concept in the Western world from Classical Antiquity until well advanced the 17th century. Disease had an Aristotelian philosophical background and a humoralist concept of the body. The causes of disease could be external or procatartic and internal or proergumenal. External causes came from natural causes: air, atmosphere, food, drinks, work, rest, sleep, vigil, secretions, excretions and mood changes. Temper and heritage determined internal causes.
The usual interpretation of disease was the humoral imbalance or corruption of humours. Diagnosis did not have the relevance it has now. The supposed triggering cause described the disease. Expressions related to excessive cold or heat, dryness or humidity, ascitis, fever and pore laxity or constriction were used. Many of the medical terms from this period remain today.
The descriptions of new diseases such as syphilis, the English sweat, gaol fever (typhus), among others, were introduced during the Renaissance and as a result of the European colonial expansion.
Rational Empiricism developed in the 17th century and is transferred to Medicine by the English physician Thomas Sydenham, who applied it to the analysis and classification of diseases. His work is the starting point for nosotaxia or classification of diseases.
In the 18th century, the development of this idea gave life to the construction of the nosological systems based on the botanical classification of Linnaeus
In the 19th century, the anatomical pathology research and analytic experiments transformed science and medical practice turning back into clinical observation of both patient and dissection and brought new methods of physical diagnosis and research. Demographic changes and new social and working conditions arising from the First Industrial Revolution marked a dramatic increase of infectious diseases due to poor urban hygiene and sanitary conditions and mass migration from rural areas into the cities. This epidemiological change demanded new hospital facilities that could enable clinical observation and practice of necropsy.
Demographic changes and new social and working conditions arising from the First Industrial Revolution marked a dramatic increase of infectious diseases due to poor urban hygiene and sanitary conditions
The French revolution ended with the old institutions and allowed medicine to reach its maximum splendour at the hospitals in Paris. A new era based on the pathological sign had started.
In the first half of the 19th century, following the Paris Clinical School, the birth of Anatomical Pathology took place, a significant event for the development of Pathology and Therapeutics. Auscultation and percussion techniques along with radiology and endoscopy were developed. New diagnostic methods based on morphological changes showed up. The lesion becomes the element to define clinical diagnosis by referring to the local changes caused by the disease.
| When | What | Who |
|---|---|---|
| 460 BC | Set base on objective observation | Hippocrates, Greece |
| 130 AD | First knowledge of anatomy, physiology and pharmacology | Galen, Italy |
| 910 | First to identify smallpox | Rhazes, Persia |
| 1249 | Invention of glasses | Roger Bacon, United Kingdom |
| 1302 | First legal autopsy | University of Bologna |
| 1590 | Invention of microscope | Zacharius Jannssen, Holland |
| 1670 | Discovery of blood cells | Anton van Leeuwenhoek, Belgium |
| 1816 | Invention of stethoscope | René Laënnec, France |
| 1818 | First blood transfusion | James Blundell, United Kingdom |
| 1844 | First use of anaesthetic | Horace Wells, USA |
| 1849 | First woman to receive a medical degree | Elisabeth Blackwell, USA |
| 1852 | First hemocytometry | Karl von Vierordt, Germany |
| 1864 | First blood transfusion | Roussel, France and Aveling, United Kingdom |
| 1869 | First glass hypodermic syringe | Hermann Wülfing Luer, Germany |
| 1877 | First contact lenses | Adolf E. Fick, Switzerland |
| 1882 | First vaccine for rabies | Louis Pasteur, France |
| 1890 | First vaccine for tetanus and diphtheria | Emil von Behering, Prussia |
| 1890 | First Clinical laboratory | London, United Kingdom |
| 1895 | Discovery of X-rays | Wilhelm Conrad Roetgen, Germany |
| 1897 | First commercial clinical laboratory | United Kingdom |
| 1899 | Aspirin is developed (original from willow tree bark and used since 400 BC to relieve pain) | Felix Hoffman, Germany |
| 1901 | ABO blood typing | Karl Landsteiner, Austria |
| 1912 | First treatment with insulin | Issued for treating diabetes |
| 1913 | Development of electrocardiograph | Paul Dubley White, USA |
| 1927 | First vaccine for tuberculosis | Albert Calmette and Jean Marie Camille Guerin, France |
| 1928 | Penicillin is developed | Alexander Fleming, United Kingdom |
| 1935 | First use of extracorporeal circulation | John H. Gibbon, USA |
| 1937 | First blood bank | Bernard Fantus, USA |
| 1945 | First vaccine for influenza | Macfarlane Burnet, Australia |
| 1950 | Invention of the first cardiac peacemaker | John Hopps, Canada |
| 1953 | Description of the structure of DNA molecule | James Watson and Francis Crick, United Kingdom |
| 1954 | First kidney transplant | Joseph Edward Murray, USA |
| 1964 | First vaccine for mumps | Jeryl Lynn, USA |
| 1967 | First heart transplant | Christian Barnard, South Africa |
| 1978 | First test-tube baby | Patrick Steptoe and Robert Edwards, United Kingdom |
| 1983 | HIV/AIDS identified | Robert Gallo, USA and Luc Montagner, France |
| 1996 | Dolly the sheep | First mammal cloned |
| 1998 | Discovery of stem cells | Thomson et al and Gearhart et al, USA |
In mid 19th century, laboratory medicine is born, focusing the explanation of the states of disease on the concept of dysfunction. As a result of this new approach comes the experimental pathology which tries to apply this experimental method to the explanation of the origin and development of disease. The search for signs of functional impairment generates the use of tests to seek for functional performance, such as liver, kidney or respiratory function tests. This situation favours technical development creating a number of instruments to evaluate functional state and metabolic function and chemical tests for body fluids. Disease is no longer a local event but an ongoing and measurable process.
Medical developments have substantially modified the traditional physician-patient relationship and the view of a patient as a person
In late 19th century, the animal infection transmission is discovered. Bacteriology is born with two important precursors of modern microbiology, Luois Pasteur and Robert Kock.
In the 20th century, lab tests became the main tool to define health and disease criteria by normal biological patterns. In case of internal origin disease or caused by the body, the scientific explanation of pathological inheritance or inherited transmission of certain diseases started providing answers to processes previously considered mysterious to medicine and were subject to speculation.
In the second half of the 20th century, conventional radiology began to be used consistently as a diagnostic support to lab tests. The development of new radiological techniques, such as computerized tomography, have introduced a new independent diagnostic line, diagnostic imaging. At the end of this century, another new technique bursts in: the magnetic resonance. A higher resolution with no ionizing radiation boosted its race for developing new techniques that could improve diagnostic tests sensitivity and specificity, optimizing quality and timing. In the last few years, ultrasound, Doppler, positron emission tomography and photon emission tomography have joined, enabling physicians to visualize the body in ways that would have been considered almost a miracle less than a generation ago.
All these developments have substantially modified the traditional physician-patient relationship and the view of a patient as a person. The quick progress and development of the specialty of diagnostic imaging lead to a constant improvement of equipment, innovative technological applications, clinical and scientific maturity of the already involved radiologists and increased interest of other physicians on the value of the provided information. Advances in technology have allowed us making a diagnosis that was previously impossible. An enormous amount of elusive pathology is now available for research thanks to modern technology.
Health and illness throughout history
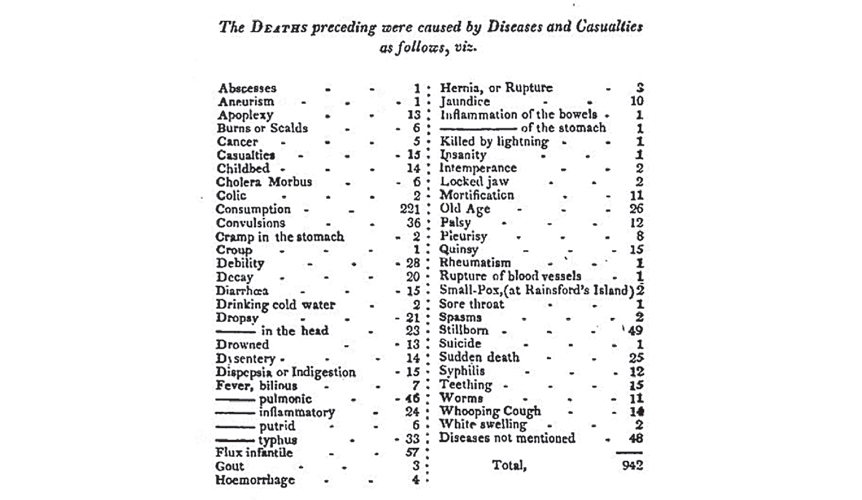
Mortality studies establish the technical principles and diagnostic expressions used by physicians at every stage of history. Moreover, they help us understand the concepts of health and illness at all times.
In the 19th century, diagnostic tools, including the microscope and X-ray, helped provide hard data independent of subjective judgement and anecdote
One of the main difficulties in historical health care data reconstruction, more specifically on causes of death, is in the diagnostic expressions used at the time since most of them do not match with any current classification. We must take into account that there was hardly any access to a physician or medical treatment and the parish or civil register did the registration of the cause of death, frequently done by someone either lacking of any medical knowledge or using popular expressions that had no direct relationship with the real cause of death. Cannonballs, war injuries and pandemics are described as cause of death throughout history. It is not until the 19th century when the first records of cause of death in the population can be found. Teething stands out as the main cause of death in infants below the age of 5. This term refers to drooling when teething, which disappears when the process is over. The disease is present when dribble gets inside and therefore it must be taken out. This shows popular practice, attitudes, ideas and beliefs not participated at all by physicians.
In the United States, one of the first bills of mortality is from the Town of Boston. The main cause of death was tuberculosis, so then called “consumption” due to the consumption of body tissues caused by the infection.
The most frequent causes of death from table 3 are:
- Consumption or tuberculosis.
- Flux infantile.
- Stillborn.
- Diseases not mentioned.
- Pulmonic fever.
- Convulsions.
- Typhus.
- Old age.
- Sudden death.
| Inflammation | Pneumonia |
| Teething | Nerve impairment |
| Fever | Tysis |
| Irritation | Diarrhoea |
| Measles | Cholera |
| Bronchitis | Lockjaw |
| Apoplexy | Malaria |
| Congestion | Smallpox |
Abstract of the Bill of Mortality for the Town of Boston.
Thanks to development of medicine, the disease gathers its own identity and is defined by itself not by its symptoms.
The evolution of diseases is shown in table 4 with the comparison of the top 10 causes of death in 1900 vs 2000 published by the US Centre for Disease Control and Prevention.
| 1900 | 2000 |
|---|---|
| Pneumonia | Heart disease |
| Tuberculosis | Cancer |
| Diarrhoea | Cerebrovascular disease |
| Heart disease | Respiratory diseases |
| Cerebrovascular disease | Accidents |
| Liver disease | Diabetes |
| Accidents | Pneumonia / Influenza |
| Cancer | Alzheimer |
| Age/ natural aging | Kidney disease |
| Diphtheria | Blood disorders |
Following this evolution, in 1900 we can see how infectious diseases are no longer the main causes of death and other impairments better defined by new technology are showing up. As economy improved, so did Public Health with the extension of sewage system for waste water collection, domestic water supply and scientific research outcomes with vaccination programs, treatment with antibiotics, the development of new diagnostic techniques and discovery of new diseases.
Health and country income
Teething was considered a disease, showing popular practice, attitudes, ideas and beliefs not participated at all by physicians
The best example of the evolution of the concept of health is in the mortality rates published by the WHO (World Health Organization), ranking causes of death by country income. This classification shows the intimate relationship between the concept of health and illness and the society we are living in.
Table 5 shows the top 10 leading causes of death nowadays. Countries are grouped according to the World Bank classification by country income. Last column refers to the global situation (Global-World).
| Low-Income | Middle-Income | High-Income | Global-World |
|---|---|---|---|
| Lower respiratory infections | Ischaemic heart disease | Ischaemic heart disease | Ischaemic heart disease |
| Diarrhoeal diseases | Stroke and other cerebrovascular disease | Stroke and other cerebrovascular disease | Stroke and other cerebrovascular disease |
| HIV/AIDS | Chronic obstructive pulmonary disease | Trachea, bronchus, lung cancers | Lower respiratory infections |
| Ischaemic heart disease | Lower respiratory infections | Alzheimer and other dementias | Chronic obstructive pulmonary disease |
| Malaria | Diarrhoeal diseases | Lower respiratory infections | Diarrhoeal diseases |
| Stroke and other cerebrovascular disease | HIV/AIDS | Chronic obstructive pulmonary disease | HIV/AIDS |
| Tuberculosis | Road traffic accidents | Colon and rectum cancer | Trachea, bronchus, lung cancers |
| Prematurity and low birth weight | Tuberculosis | Diabetes | Tuberculosis |
| Birth asphyxia and birth trauma | Diabetes | Hypertensive heart disease | Diabetes |
| Neonatal infections | Hypertensive heart disease | Breast cancer | Road traffic accidents |
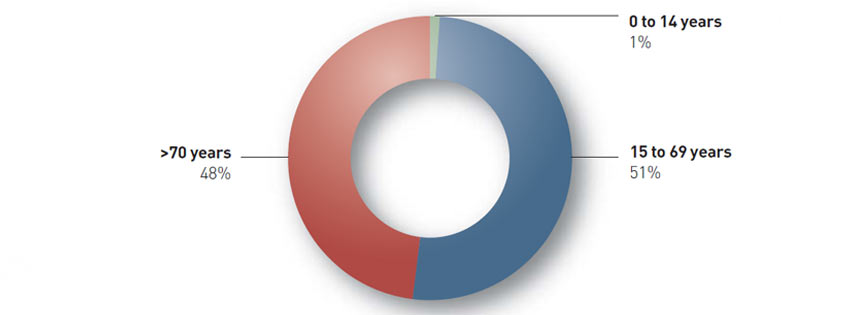
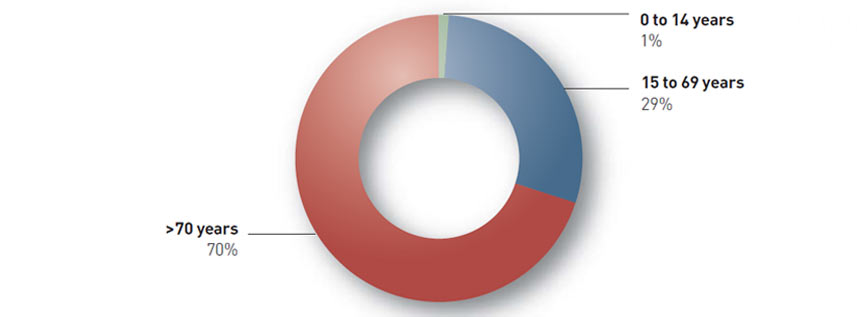
From the analysis of the distribution of deaths per age group, we can find that:
- In low-income countries, less than a fourth of all people reach the age of 70 and more than a third of all deaths are among children below the age of 14. Infectious diseases such as lung infections, diarrhoeal diseases, HIV/AIDS, tuberculosis, and malaria claim many lives in these countries. Complications of pregnancy and childbirth together continue to be leading causes of death, claiming the lives of both infants and mothers.
- In middle-income countries, nearly half of all people live to the age of 70 and chronic diseases are the major killers, just as they are in high-income countries. Unlike in high-income countries, however, tuberculosis, HIV/ AIDS and road traffic accidents also are leading causes of death.
- In high-income countries, more than two thirds of all people live beyond the age of 70 and predominantly die of chronic diseases: cardiovascular disease, chronic obstructive lung disease, cancers, diabetes or dementia. Lung infection remains the only leading infectious cause of death.
Source: World Health Organization (WHO) 2011.
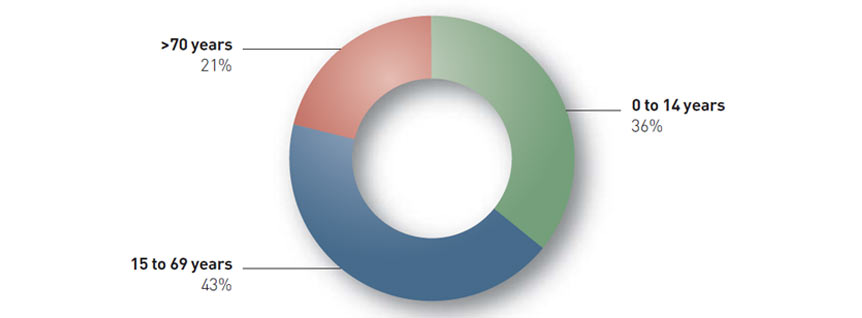
Source: World Health Organization (WHO) 2011.
Source: World Health Organization (WHO) 2011.
Modern Medicine
Modern medicine not only applies these technology advances to treating diseases but also learns from medical and epidemiological statistics to evaluate healthcare policies and encourages scientific research.
In industrialized countries, infections are no longer the leading cause of death; however, there are other social habits greatly affecting the health of the population.
Tobacco use is a major cause of many of the world’s top killer diseases, including cardiovascular disease, chronic obstructive lung disease and lung cancer. It is responsible for the death of almost one in 10 adults worldwide. Smoking is often the hidden cause of the disease reported as responsible for death.
The analysis of the molecular concepts links mechanisms, pathways and pathologies
Cardiovascular diseases kill more people each year than any others. In 2004, 7.2 million people died of ischaemic heart disease, 5.7 million from stroke or another form of cerebrovascular disease.
Current concept of health includes giving up habits and causing a negative effect on our life expectancy. We seek to live better and longer.
Modern medicine not only uses advanced technology for diagnosis and treatment but also applies scientific knowledge to the definition of disease. It is getting further from the external sign to dig in the behaviour of the molecules taking part in cells. The analysis of the molecular concepts links mechanisms, pathways and pathologies, such as cancer. Gene expression analysis leads to identify molecular subtypes related to certain outcomes or cell expression. The identification of certain genes expressed in certain types of cancer and the response to certain cancer treatments, the inhibition or activation of enzyme precursors that alter hormone production or the presence of cell membrane receptors represent the new concept of disease. We look for molecular alterations to work at this level to avoid the external symptoms that once described the disease causing death. Maybe, in the near future, diarrhoea will be a simple interleukin imbalance causing inflammation to alter the Na/K pump, thus creating a molecular imbalance causing contraction of colon muscular fibres and closing of cell channels.
Most likely Galen would have identified these molecular changes as humoral changes, as in his teachings.
How did medical knowledge fit in the development of insurance?
The first serious attempt to establish population mortality rates was made by John Graunt, a London draper’s son, who analyzed the records of the christenings and burials in the City of London in his spare time, periodically published since the plague in 1603. In 1662, Graunt published a book called “Natural and Political Observations made upon the Bills of Mortality”. From this information he compiled a “Table of survivors”, which was to be a model for subsequent life tables.
Some years later, Edmund Halley, an astronomer, published an essay “An Estimate of the Degrees of Mortality of Mankind drawn from Curious Tables of the Births at the city of Breslaw”. It was the first work by a competent scientist using reasoning up-to-date statistics.
Although Halley’s work, along with that of Newton and De Moivre, laid the foundation of actuarial science, it was not until the next generation that James Dobson, De Moivre’s pupil, showed in 1756 that life assurance was practicable with premiums graduated according to age.
The passing of the Life Assurance Act by Parliament in 1774 did away with many of the old abuses, such as speculation on lives of other by people who had no real interest in those lives.
In 1837, the registration of births, marriages and deaths became compulsory in England, which enabled the development of the first official English life table in 1843.
In the earliest days of life insurance, it used to be sufficient for a candidate to appear before the board of directors, who assessed the candidate’s health
At the other side of the Atlantic, the USA life insurance developed in a similar manner to that in England. It was not until 1809, in Philadelphia, that the Pennsylvania Company for Insurance and Granting of Annuities started selling life insurance on strictly commercial basis. Its most important contribution was the innovation in its underwriting practice with the requirement of an application or proposal and a medical examination. Premiums were based on the age of the applicant. In 1823, the Massachusetts Hospital Life Insurance Company introduced a rate book.
Life business at the beginning of the 19th century existed mainly to facilitate commerce and was very restricted. It was not until the 1840s that the industry was given a boost.
In the earliest days of life insurance, it used to be sufficient for a candidate to appear before the board of directors, who assessed the candidate’s health. Later on, a physician was invited to sit with and advice the directors on the state of health. As the volume of life business grew, a system of medical examination evolved. The practice started in the United States but it was not established in Great Britain until some time before the middle of the century.
In view of the technical requirements involved in medical selection, ALIMDA or Association of Life Insurance Medical Directors of America was founded in North America in 1889. In 1991 this association decided to change its name to the American Academy of Insurance Medicine, AAIM. It holds a worldwide known annual meeting. In England, the Assurance Medical Society was founded in 1893 holding evening meetings three times every year in London. Since 1985, the society has held biennial meetings in the UK jointly with the Institute of Actuaries.
The first International Congress for life assurance was held in Brussels in 1899. In 1931 a permanent international committee and a Bureau was set up to organize a congress every three years. The first official International Congress for Insurance Medicine was held in London in 1935, giving rise to ICLAM, International Committee for Insurance Medicine. Since then, this organization brings together medical experts, actuaries, lawyers and underwriters, holding a conference every three years in different parts of the world. Next May 2013, Madrid will hold its twentyfourth edition. This forum will discuss medical issues related to life, disability, dependency, health and accident insurance.
The medical examination first started checking blood pressure, height & weight, and the lack of infectious diseases; later on, a medical questionnaire inquiring about the health status of the applicant through a set of questions was added. At the beginning of the 20th century laboratory testing is included, mainly to identify unknown or unreported diabetes and renal diseases. Years later X-rays joined and later on stress testing. In the last decade, echocardiography and Doppler echocardiography have become part of the testing for high sum assured.
Laboratory testing has not only evolved in quality and techniques but has developed three categories within risk assessment:
- Screening tests to find undisclosed conditions or identity use of substances such as cocaine, nicotine or alcohol.
- Reflex tests to control a follow-up of a disclosed impairment or rule out a transitory condition. Glycosylated haemoglobin is a good example. It shows how well the diabetes is under control or a temporary raise in blood sugar, which does not imply any additional risk.
- Test for cause are ordered based on a disclosed condition that requires additional information, usually ordered by Medical Directors or Advisors.
In the last 20 years, alternative testing to traditional blood tests have developed, mainly related to low sum assured.
Oral fluid testing or saliva test are a fast and inexpensive way to identify the presence of HIV, use of substances or smoking
Oral fluid testing or saliva test are a fast and inexpensive way to identify the presence of HIV, use of substances or smoking. It is important to mention that a positive response in any fluid or oral tests must be confirmed with a blood test. Some other tests for different parameters were developed but never were as successful as those used for HIV infection and the use of drugs. Insurance products with low sum make use of this fast and inexpensive test.
The medical questionnaire has also evolved, not only due to medical advances but also to new technologies and process cost.
The introduction of internet and rapid expansion of information technology have changed the process for gathering information about health status.
Problems such as the limited number of questions or cumbersome wording, which make it difficult for disclosing certain conditions, together with new distribution channels, have helped the development of expert systems for automated decision-making process and health questionnaires.
Expert systems contribute with diagnostic algorithms where a large amount of data is input, as in medical practice. Expert systems in risk assessments make easier the design of precise questionnaires, capable of gathering lots of additional information or even come up with a rating.
Tobacco use is a major cause of many of the world’s top killer diseases including cardiovascular disease, chronic obstructive lung disease and lung cancer. It is responsible for the death of one in 10 adults worldwide
Last point to mention is the strong push diagnostic imaging is getting, especially in the area of cardiovascular. The ability to visualize the blood flow in the heart and precisely evaluate any stenosis makes us re-evaluate the use of other diagnostic techniques, such as stress testing.
It is also true that today the cost of this imaging technology is high but one cannot forget that other techniques were also expensive at their time and cost came down as use increased.
Market pressure to increase non-medical limits together with the continuous improvement of information technology are pushing to implement a risk selection process based more on the candidate’s knowledge of his/her health and the use of specific tests based on the answer.
Reminder
Men and women live longer thanks to technical advances and scientific research. We must not forget that we want to live longer and better. To achieve this goal we must commit ourselves to improve health care. Luckily, we live in a time where living conditions are very nice despite the difficult economical times we face. Our duty is to cooperate with HealthCare policies that help us maintain a healthy lifestyle and prevent disease.
Bibliography
Advances in Medical technology at http://timecoast.com
Biomarkers Unbound - The Supreme Court’s
Ruling on Diagnostic - Test Patents.
NEJM 366; 25 NEJM 2338 org June 21, 2012.
Most frequent diseases at the beginning of the
19th century and their treatment.
Las enfermedades más frecuentes a principios
del siglo XIX y sus tratamientos.
Enrique
de la Figuera von Wichmann, President
of the College of Physicians in Zaragoza, Los
Sitios de Zaragoza. Alimentación, enfermedad,
salud y propaganda, IFC 2009.
Baron Duffy, M.L. (2003). New Jersey Health Statistics, 2000. Trenton, NJ: New Jersey Department of Health and Senior Services, Center for Health Statistics. http://www.state.nj.us/health/chs/stats00/index.html
Board of Health of the State of New Jersey
(1901).
Twenty-Fourth Annual Report of the Board of Health
of the State of New Jersey and Report of the Bureau
of Vital Statistics, 1900. Trenton, NJ: The John L.
Murphy Publishing Co.
Integrating modern and traditional medicine:
Facts and figures.
Priya Shetty , 30 June 2010.
The Burden of Disease and the Changing Task
of Medicine.
David S. Jones, M.D., Ph.D., Scott H. Podolsky,
M.D., and Jeremy A. Greene, M.D., Ph.D. NEJM
366;25 june 21, 2012.
Historical analysis of causes of death.
Problems and solutions.
El análisis histórico de la mortalidad por causas.
Problemas y soluciones.
Revista de Demografía histórica XXI, I, 2003,
segunda época. José Bernabeu Mestre, Diego
Ramiro Fariñas, Alberto Sanz –Gimeno y Elena
Robles Gonzalez.
Causes of death and relationship between
scientific knowledge and popular knowledge.
Causas de muerte y relación entre conocimiento
científico y conocimiento popular.
Revista de Demografía Histórica, Enrique Perdiguero
Gil. ISSN 1696-702X, Vol. 11, Nº 3, 1993.
Medical theories and classification of cause
of death.
Teorias Médicas y la clasificación de las causas
de muerte.
Josep Lluis Barona. Revista de Demografía
Histórica, ISSN 1696-702X, Vol.11, Nº3, 1993.
A brief history of medical diagnosis and the
birth of the clinical laboratory.
Darlene Berger, July 1999,
www.mlo-online.com
Brakenridge’s Medical Selection of Life Risks.
Fifth edition. Ed Palgrave. Macmillan, 2006.



