Lifestyle, what is there behind the word?Personal
Ana Luisa Villanueva
Chief Medical Officer Life, Health & Accidents MAPFRE RE
Madrid - Spain




Finding out the meaning for Lifestyle is not an easy task since it mirrors one’s attitudes and values towards life. The prestigious Spanish cardiologist, Dr. Valentin Fuster, in his book “Promoting cardiovascular heath” expressed a splendid idea on what counts for the individual when deciding on a lifestyle.
First level Factors
- Determinants: ranging from globalization of our society to education and cultural and social rules through the social model and healthcare system.
- Political approach: ranging from an international to a national or local perspective involving financial, legal, regulatory and trading issues.
- Healthcare system: including system infrastructure, access to care, quality of care, drugs, technology and heath workforce.
- Communication: health communication through Media, Community interventions or settings based.
Second level Factors
- Determinants: divided into biological and behavioural risk.
- Political approach: creating the environment to enable individuals to make and maintain healthy choices.
- Healthcare system: delivering preventive care and rehabilitation services as well as diagnostic and therapeutic.
- Communication: enhancing knowledge, motivation and individual’s skills.
Third level factors
These factors are framed on the more intimate individual’s environment, the society he or she lives in and is identified with, his/ her community, neighbourhood, family and friends.
Primordial prevention refers to a healthy lifestyle that does not permit risk factors to appear, mainly those for cardiovascular disease
This approach may seem overly bureaucratic and impractical when it comes to health; however, it will not only depend on genetic background but on one’s lifestyle.
The consequences of such decision are not only obvious to the individual who will enjoy a better or worse health but will provide some feedback to the environment, changing those factors influencing primary choice.
Lifestyle is shown at first glance, the way you dress, the attitude towards life, the way you work, your relationships with others, the way you take healthcare, your beliefs, the way you think, your likes, your leisure preferences and eating habits.

The American example
When bringing Lifestyle into health, we find that for the American Heart Association – AHA, a healthy Lifestyle consists of sufficient exercise, a superior diet score, absence of smoking and a BMI (Body Mass Index) ≤25 kg/m2.
They also define ideal health factors as untreated normal values of blood pressure, cholesterol and fasting glucose, being the main risk factors:
- Alteration in lipid profile or dyslipidemia.
- High blood pressure.
- Diabetes.
At age 50 the absence of traditional risk factors is associated with extremely low lifetime risk and significantly greater longevity
Here are some overwhelming facts published by the Cardiometabolic Research Institute, at Houston (Texas), which mention that:
- Nearly 70% of adult Americans are overweight or obese; the prevalence of visceral obesity stands at 53% and continues to rise. At any one time, 55% of the population is on a weight-loss diet, and almost all fail.
- Fewer than 15% of adults or children exercise sufficiently, and over 60% engage in no vigorous activity. Among adults, 11%– 13% have diabetes, 34% have hypertension, 36% have prehypertension, 36% have prediabetes, 12% have both prediabetes and prehypertension, and 15% of the population with either, diabetes, hypertension, or dyslipidemia is undiagnosed. About onethird of the adult population, and 80% of the obese, have fatty livers.
- With 34% of children overweight or obese, prevalence having doubled in just a few years, type 2 diabetes, hypertension, dyslipidemia, and fatty livers in children are at their highest levels ever.
- Half of adults have at least one cardiovascular risk factor. Up to 65% of patients do not have their conventional risk biomarkers under control. Perhaps it is even more shocking to see the poor patient adherence to treatment, typically below 50%.
- The same source reveals a similar situation worldwide, with the prevalence of metabolic syndrome (presence of a number of altered factors: glucose, blood pressure, HDL, waist and triglycerides) approaching 50%.
The result from its reading is primordial prevention, referred to as healthful lifestyle habits that do not permit the appearance of risk factors, mainly those of cardiovascular risk.
Diagnostic tools used in cardiovascular risk
- Clinical evaluation: history and physical examination.
- Family history.
- Global Risk scoring.
- Lifetime Risk Calculator.
- ECG - Electrocardiogram.
- Echocardiography.
- Stress testing or ergometry.
- MPI –Myocardial perfusion imaging.
- LDL-C -apolipoprotein B, non-HDL-C.
- HDL-C.
- Lipoprotein “little a” (Lp(a)).
- Lipoprotein fractionation (VAP, NMR).
- CRP hsC-reactive protein.
- Lipoprotein-associated phospholipase A2 (Lp-PLA2).
- Coronary angiography.
- CIMT Carotid intimamedia thickness using ultrasound.
- CAC Computed tomography for coronary calcium.
- CT coronary angiography.
- MRI coronary angiography.

Unfortunately, most coronary heart disease (CHD) events arise in a large subpopulation of low to moderate risk individuals, therefore the challenge remains at prevention and identification of the disease at this level.
There is also some good news, at age 50 the absence of traditional risk factors is associated with extremely low lifetime risk and significantly greater longevity.
A combination of approaches such as primordial prevention and refinement of risk prediction, guideline compliance, novel treatments, improvement in adherence, and preventive policies, will be necessary to lower the present high risk burden.
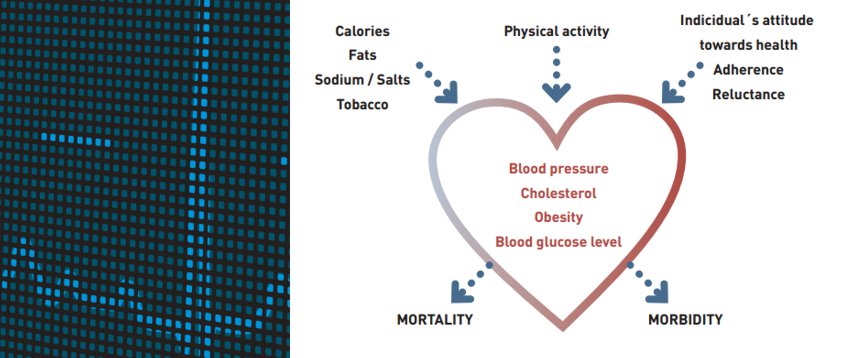
Most risk factors that drive cardiovascular disease have genetic, physiologic, behavioral, and environmental components. Among them there are non modifiable risk factors including age, genetics, and gender but other modifiable risk factors comprising smoking, eating habits (fats raising cholesterol, sugar and salt intake) and weight gain.
Non-traditional Risk Factors
The above factors have been considered as traditional risk factors up to date. However, there are emerging or novel risk factors called non-traditional factors including:
- Blood test:
- CRP – C-reactive protein.
- Lp-PLA2- lipoprotein-associated phospholipase A2.
- LDL-P - LDL particle number.
- Fibrinogen.
- Lpa - Lipoprotein a.
- TG - triglycerides and triglyceride-enriched particles.
- PAI-1 plasminogen activator inhibitor.
- IL-6 – Interleukin 6.
- Imaging techniques capable of refining risk
prediction or improving management:
- CIMT-Carotid ultrasound to measure carotid intimamedia thickness.
- CAC- Coronary artery calcification.
- MRI – Magnetic Resonance Imaging.
- CT – Coronary angiography.
Prevention: goals and methods
Prevention, although relatively unfashionable when compared to cuttingedge hightech procedures, addresses three goals of medicine:
- Preventing disease.
- Relief of suffering.
- Prolonging life.
The prevention may generally refer to screening and immunizations to detect, forestall, or limit serious disease.
The Mediterranean diet includes most of the “Life’s Simple 7” but some of these parameters refer to the individual’s attitude towards healthy life style
If cardiovascular disease is taken as an example, Primary prevention denotes delaying or limiting a first event in individuals who have not yet been formally diagnosed with disease. The identifying risk factors are commonly regarded as if they were in fact a reason for an initial therapy. Secondary prevention seeks to prevent, postpone, or limit recurrence of a clinical event in patients who have been previously diagnosed with disease.
Unfortunately, the functional distinction between types of prevention appears to be blurring thus generating costineffectiveness when allocating budgets for Preventive Medicine. The National Institute for Health and Clinical Excellence (NICE) in the UK estimated that a 1% population wide lowering of cardiac risk factors would net substantial savings yet even with prevention services remaining as they currently are.
“Life’s Simple 7” defined by the American Heart Association
- Not smoking or quitting over 1 year ago.
- Body Mass Index BMI ≤25 kg/m2.
- Exercising at a moderate intensity for ≥150 minutes or 75 minutes at vigorous intensity each week.
- Eating a “healthy diet”: adhering to 4 to 5 important dietary
components
- Sodium intake < 1,5 g/day.
- Sugarsweetened beverage intake ,36 oz or < 1 liter weekly.
- 4 to 5 pieces of fruit or 4.5 cups and vegetables per day.
- Three 1 oz servings or ≥6 spoons of fiberrich whole grains per day.
- Two 3.5 oz servings of oily fish or 250 mg per week.
- Maintaining total cholesterol (TC) < 200 mg/dL.
- Keeping blood pressure ≤120/80 mmHg.
- Keeping fasting blood glucose < 100 mg/dL.
“Life’s Simple 7”
The American Heart Association - AHA has defined ideal cardiovascular health with a list of 7 parameters including four related to behaviour and 3 factors for control.
Obviously, the list should follow the eating habits of each part of the world. Fortunately, the Mediterranean diet already includes most of the points mentioned above, not to forget that the rest of these parameters refer to the individual’s attitude towards healthy living.
Health Status: therapy and behaviour
Now let’s fit lifestyle into the three health status:
- Disease has been diagnosed.
- Subclinical disease.
- Disease does not exist.
The three of them share some risk factors:
- Level of exercise or physical activity.
- Obesity.
- Aging: cutoff point at age 55 for males and 60 for females.
- Tobacco / smoking.
The three of them should check the same parameters:
- Glucose.
- Blood pressure.
- Cholesterol.
All three are very much influenced by the individual’s environment and attitude towards health. The patient level of adherence to prescribed medication is of high importance to keep in line the parameters above. It is as well essential for Health Care Delivery to have means to monitor the follow up and provide enough resources, costly-effective, to reduce both mortality and the use of health services.
The pharmaceutical industry is now involved in the development of a new concept of pill. Coronary heart disease represents the biggest challenge to society. Patients are forced to take several pills to control their disease. Substituting all of them for just one, the so called polypill, will not only change cost of treatment but improve patient approach to disease, increasing adherence and follow-up.
When the disease is subclinical, such as in treated hypertension with normal blood pressure readings and no other events, the patient attitude is critical. Control of risk factors together with appropriate monitoring greatly decreases mortality risk.
The use of inexpensive, non invasive techniques such as CIMT, carotid intima-media thickness imaging for cardiovascular diseases or biomarkers in brain degeneration helps predict risk of disease events that have not yet occurred.
Promoting Health in our society
Patient adherence to prescribed medication is vital as well as costadjusted follow-up health care plans
Influenced by:
Behaviour. We live in a consumer society where there is no frustration tolerance. We are used to have and get everything we want. Stress is generated when not achieving all we crave, thus creating an unnecessary disease. Our attitude towards life, our lifestyle is crucial to address the natural aging process. Smoking, excessive alcohol consumption, no body and mind exercise, being influenced by consumer advertising pushing for constant competition do not help for an adequate care of our health.
Lack of adequate policies. There is no sense of the lack of health promotion, which means a disease in the long term, of who invests in the project, who controls it and who gets the benefits. Doing a superficial analysis, one could say society is the one getting all benefits by improving health. However, that is not entirely true because the better the health state, the lower the costs of Health Care. The concept shifts from therapeutic cost to preventive and diagnostic cost. Even so, the investor does not offset the investment since benefits are not immediate or in the short run but in the long run.
Lack of intersectorial cooperation. Participation of the different players and work groups is required to change lifestyle. Working with the same goal at different levels makes the outcome turn into a common benefit. Just as we are becoming aware of the consequences of climate change and working on marketing campaigns to encourage a reasonable consumption of resources, we should realize that deterioration of our heath involves further care needs that could end up collapsing the current HealthCare system. Increased longevity with multiple impairments is not the same as longevity with a health state under control and identified needs.
Mixture of Health communication and Healthcare Delivery. We should be able to communicate what healthy living is and provide means to promote health. The development of marketing campaigns to improve our lifestyle must come with a commitment, at the highest level, to make the means available to meet the standards. Vaccination campaigns at school sites instead of other health centres, easy access to regular check-up for age-adjusted risk factors, non invasive diagnostic methods or hightech procedures that when applied in large population bring cost down and allows a widespread use. Obviously, all this implies providing the means for such Health Care.
Lifestyle and Insurance
Now we transfer these concepts into Insurance. So far lifestyle was limited to simple question on sports, alcohol and drug consumption, smoking, and occasionally motorcycling.
It is true that these questions provide important information on individual’s behaviour but, by no means, show the overall concept of lifestyle. We cannot monopolize the health questionnaire with questions trying to find the applicant’s vision on the point.
Perhaps a different approach to the analysis of data provided by the candidate should be considered in risk assessment.
Of course, we should ask about alcohol consumption or smoking but maybe, some other information on daily living, such as use of public transport, distance from home to workplace, eating habits (home made food, daily menu, sandwiches), sweetened drinks, sodas, leisure activities including time spent in front of the television, could be added.
Regarding health state, questions have a more specific reply:
- If disease has been diagnosed, monitoring treatment and follow-up on events are key factors. Adherence to therapy is critical for mortality and morbidity control as already mentioned.
- In case of subclinical disease, with no symptoms, follow-up, regular blood tests, changes in medication and additional testing are excellent ways to decrease mortality and morbidity.
- If there is no disease, prevention plays a key role. Regular check-ups/ routine screening adjusted to age and family history shows the way to maintain good health.
So, there are two ways for finding out the lifestyle of the individual:
- The health questionnaire.
- Medical tests.
The polypill not only changes the cost of treatment but improves patient approach to disease increasing adherence and follow-up
Understanding this approach to life will only be available through a clear and concise wording of questions. At present, questionnaires are more and more limited with both dense and short questions. Expert systems, by using triggering questions, may be the key to get complete information on any particular condition the applicant may have.
The current required medical tests will undergo deep changes in the near future. The introduction of non invasive imaging techniques and biomarkers is changing the traditional concept of diagnosis and treatment. As these new tests are becoming more reasonable and affordable, there will be a progressive shift from some of them into these new more efficient ones.
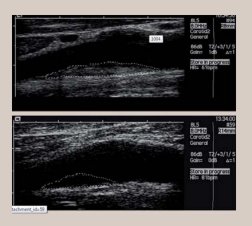
CIMT ultrasound
The CIMT ultrasound is a non-invasive test easy to use. The images below show how the atheromatous plaque is identified inside the carotid artery.
Cardiovascular accidents or strokes are one of the most common symptoms of atherosclerosis and the third leading cause of death after ischaemic heart disease and cancer. Approximately 80% of all strokes are ischaemic and 30 – 50% of these are caused by carotid atherosclerotic plaques. However, not all plaques become symptomatic and will lead to stroke. Conventionally, advanced atherosclerotic lesions are estimated to be more dangerous and internal carotid artery stenosis is considered to represent a higher risk of cerebral ischaemia when it exceeds 70 % narrowing of the lumen section.
The overwhelming majority of patients with severe carotid stenosis remain asymptomatic for years and even indefinitely. Therefore, it is self - evident that the degree of stenosis is not the only factor that represents a risk of cerebral ischaemia. Besides the degree of stenosis, the structure of the atherosclerotic plaque or pathophysiological features within the plaque increases its instability. These details play a key role in predicting stroke risk.
All these show that the vulnerable or unstable plaque has a predisposition to breaking and fissuring, and hence for embolisation to the brain or sudden occlusion of the arterial lumen, with the consequent congruent neurological symptoms.
Therefore, the use of tests such as the carotid ultrasound helps to control subclinical disease, do follow-up and make therapeutic decisions.
When disease is not present we cannot forget that we are all vulnerable and live in a society where vulnerability is poorly tolerated.
To think about
We should realize that deterioration of our heath involves further care needs that could end up collapsing the current HealthCare system
We must encourage research to move from the idea of disease into the concept of health. Motivation is implanted in our mind since childhood. The concept of lifestyle must be conveyed from the beginning of life, helping children to understand the risk factors in our system and transmitted to adults to help them change their habits.
Our attitude towards life is critical. No matter what happens, we must find a solution to keep going. We need to be consistent with our thoughts and show it in our behaviour. If things do not work as expected, an alternative plan should be considered to always look ahead.
Governments play an important role in lifestyle. Setting rules and regulations and allocating resources for Healthcare are part of this change. Regulations on food ingredients, advertising and education as well as those resources available to the public are key components for developing the lifestyle of each individual.
This change in lifestyle needs all of us to participate and involves all levels, education, communication, research, team work and attitude towards problems.
Insurance factors should think very carefully about how to include lifestyle and all it implies in the applicant’s risk assessment.

BIBLIOGRAPHY
Exercise and life expectancy Debra Efroymson, Peter Berti, Kristie Daniel The Lancet, Volume 379, Issue 9818.
Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health Valentin Fuster and Bridget B. Kelly Institute of Medicine of the national Academy of Sciences. ISBN: 0-309-14775-1.
The High-Risk Plaque Initiative: Primary Prevention of Atherothrombotic Events in the Asymptomatic Population Erling Falk & Henrik Sillesen & Pieter Munten-dam & Valentin Fuster Curr Atheroscler Rep (2011) 13:359–366.
The BioImage Study: novel approaches to risk assessment in the primary prevention of atherosclerotic cardiovascular disease--study design and objectives Muntendam P, McCall C, Sanz J, Falk E, Fuster V; High-Risk Plaque Initiative. Am Heart J. 2010 Jul;160(1):49-57.e1.
Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and Men Dariush Mozaffarian, M.D., Dr.P.H., Tao Hao, M.P.H., Eric B. Rimm, Sc.D., Walter C. Willett, M.D., Dr.P.H., and Frank B. Hu, M.D., Ph.D. N engl j med 364;25 nejm.2392 org June 23, 2011.
Primary prevention of coronary heart disease: integration of new data, evolving views, revised goals, and role of rosuvastatin in management. A comprehensive survey Drug Des Devel Ther. 2011;5:325-80. Epub 2011 Jun 13.
Lifestyle Change and Mobility in Obese Adults with Type 2 Diabetes N engl j med 366;13 nejm.org march 29, 2012.
The global obesity pandemic: shaped by global drivers and local environments Boyd A Swinburn, Gary Sacks, Kevin D Hall, Klim McPherson, Diane T Finegood, Marjory L Moodie, Steven L Gortmaker. Lancet 2011; 378: 804–14.
Health and economic burden of the projected obesity trends in the USA and the UK Y Claire Wang, Klim McPherson, Tim Marsh, Steven L Gortmaker, Martin Brown Lancet 2011; 378: 815–25
Quantification of the effect of energy imbalance on Bodyweight Kevin D Hall, Gary Sacks, Dhruva Chandramohan, Carson C Chow, Y Claire Wang, Steven L Gortmaker, Boyd A Swinburn Lancet 2011; 378: 826–37
Changing the future of obesity: science, policy, and action Steven L Gortmaker, Boyd A Swinburn, David Levy, Rob Carter, Patricia L Mabry, Diane T Finegood, Terry Huang, Tim Marsh, Marjory L Moodie Lancet 2011; 378: 838–47.
Control de los factores de riesgo coronarios y terapias basadas en la evidencia: esfuerzos coordinados para la prevención cardiovascular en España Control of Coronary Heart Disease Risk
Factors and EvidenceBased Therapies: Joint Efforts for Coronary Heart Disease Prevention in Spain Manuel Francoa, Richard Cooperc, Usama Bilala, Valentın Fuster Rev Esp Cardiol. 2011;64(11):962–964.
Lipoprotein Management in Patients With Cardiometabolic Risk: Consensus Conference Report From the American Diabetes Association and the American College of Cardiology Foundation V. Howard, James H. Stein, and Joseph L. Witztum John D. Brunzell, Michael Davidson, Curt D. Furberg, Ronald B. Goldberg, Barbara J. Am. Coll. Cardiol. 2008;51;1512-1524.
HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms Mohamad Navab, Srinivasa T. Reddy, Brian J. Van Lenten & Alan M. Fogelman Nature Reviews Cardiology 8, 222-232 (April 2011).



